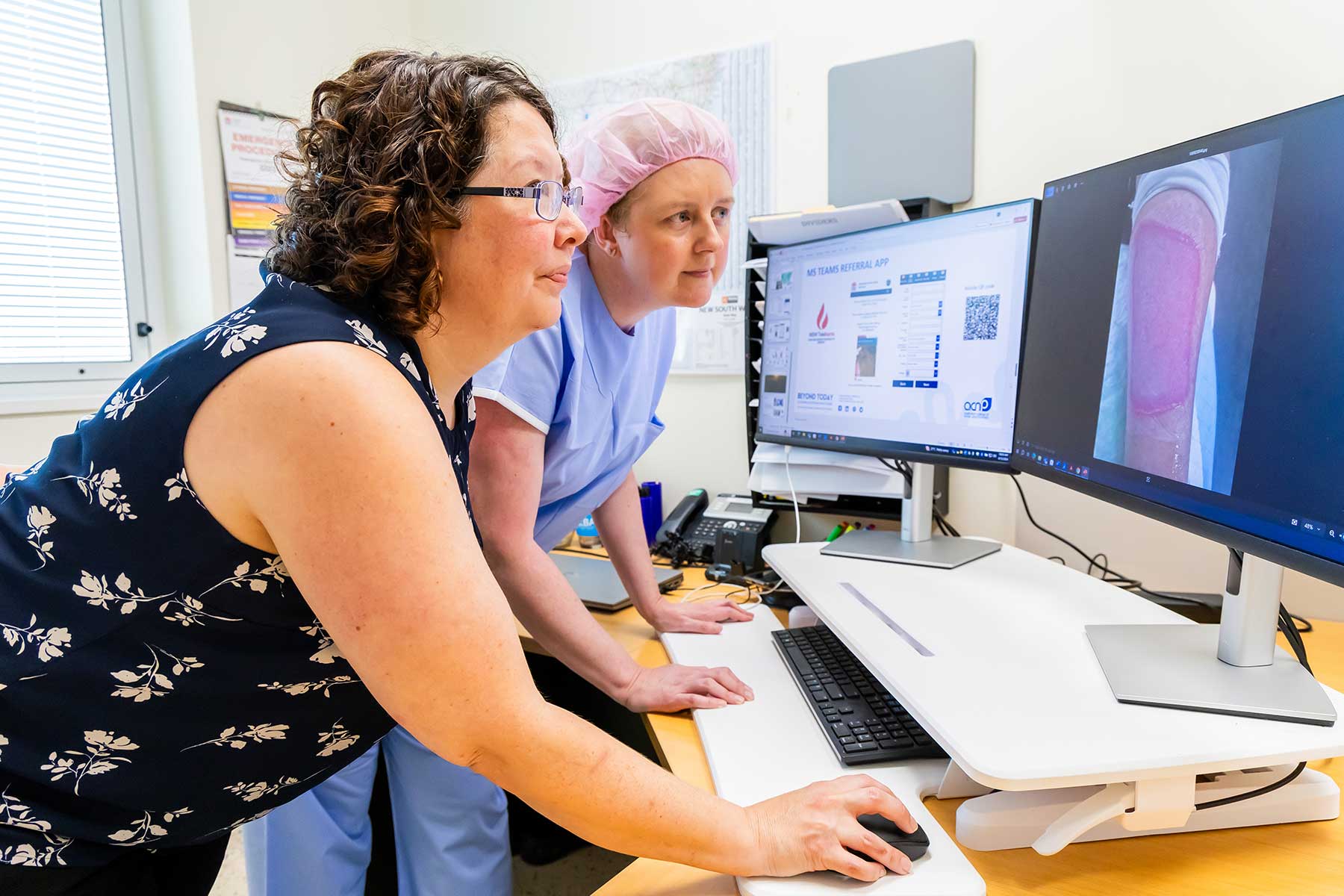
Image: NSW Teleburns Concord Hospital specialist multidisciplinary care
There are 13 burns units in Australia, all located in major metropolitan hospitals. These units each have their own rural catchment area.
Since the early 2000’s, Concord Burns Unit’s virtual burns support service has been providing specialist burns support to 11 different Local Health Districts (LHD) in NSW and the ACT. Burns rural telehealth support is available to patients with burn injuries from 218 regional and rural towns, classified as being more than two hours’ drive away from Concord. This makes up over 40 per cent of the total burns referrals to Concord Burns Unit.
Traditionally, in order to assess burn wounds in rural patients, specialist burns clinicians review digital photographs of the wound and transfer the patient to a burns unit for inpatient or outpatient treatment. Clinicians rely on these photographs to make clinical decisions or give advice, and they are generally sent via email or mobile phone, with a wide variation in image quality. Traditional video conferencing has not provided the visual quality required to make accurate clinical decisions.
In 2019, eHealth NSW partnered with Concord Burns Unit to implement NSW Teleburns. Located at Concord Repatriation General Hospital in Sydney Local Health District, it uses the statewide unified communications platform with its high-definition pan tilt zoom video camera on wheels to connect burns patients and clinicians from rural NSW to the entire multidisciplinary team at Concord.
The project was rolled out as follows:
Phase 1 of the pilot was rolled out at Griffith Hospital specialist outpatient clinic, where the technology was first trialled with patients being cared for by nursing staff.
Phase 2 of this technology was rolled out to an additional five key referral outpatient wound clinics (Wagga Wagga, Bathurst, Orange, Dubbo and Bega) in September 2022.
Phase 3 saw the development, trial and implementation of a MS Teams referral app, with guidelines, contacts, mandatory fields and the ability to upload wound images.
In phase 4, the utilisation of MedSync allowed for storage of patient wound images in the Electronic Image Repository, which allows clinicians in NSW Health to access images, irrespective of Local Health District.
During Phase 5, Medsync Connect was introduced. This provided a recordable video connection between any clinician and patient with only the need for a mobile phone and internet access. It enables optimal burns management and treatment, without the need to travel to Sydney.
The evolution of this service has led to exponential demand. In the first three years since its implementation, Concord Burns unit has seen 234 fewer admissions and supported 362 patients solely by virtual care. There have been over 2000 occasions of service per year, and it has helped ensure that all adult patients have access to optimal multidisciplinary specialist burns care, regardless of their postcode.
Another advantage to this model is that rural doctors and nurses are educated and supported in all aspects of burns care and follow-up management, increasing their knowledge and confidence in managing acute burns patients.
On average per patient, the service saves approximately 11 hours of travel time, $1680 in accommodation and the emotional distress of having to travel to Sydney. It also saves the health system a huge expense related to transport and patient admission. Rural patients can also be discharged earlier as they will be following up with the same specialists virtually.
Benefits
- Access to specialist burns care.
- Ability to observe wound bed assessment of colour, capillary refill and sensation.
- Ability to observe patient body language, movement/exercises, wound cleansing technique, dressing applications, massage techniques and pressure garment fitting.
- Improved patient/clinician relationship (compared with digital image and teleconference/email consultations).
- Education for patients, families and clinicians, for example, debridement coaching, dressing choice.
- MS teams provides data privacy and security.
Challenges
- Internet availability and reliability.
- Unintended increase in workload.
- Need for rural clinics to have and use technology.
- Slow uptake of emerging technology by health.
- Implemented solutions may not be optimal for all health areas.
- Current inability for electronic medical record access between LHDs and states.
The service has been pioneered by nurse practitioner Miranda Pye, who has been a burns clinician for over 20 years. As a nurse practitioner-led service, advantages involve the ability to order tests, diagnose, provide prescriptions, certificates and the referral of patients to other services. It is coordinated by Miranda, whose enhancements have seen the growth of this service rise approximately 1000 per cent in the past 10 years. Miranda has developed collaborative relationships between health services and hopes to expand the service even further into the future.
This article was originally published in the Spring 2025 edition of ACN’s quarterly member publication The Hive. Members can access all past editions of The Hive on MyACN. Non-members can get a sneak peek by viewing our open-access articles.
Author: Miranda Pye
Nurse Practitioner, Concord Repatriation General Hospital

Author: Melissa O’Loughlin MACN
ACN Nurse Educator – Higher Education